Eligibility in Benzene exposure cases is usually driven by two questions:
- Whether toxic exposure can be reasonably documented,
- Whether a medically supported diagnosis links that exposure to serious health conditions.
Benzene is widely treated as a high-priority hazard because it is a proven blood and bone-marrow toxicant, and federal public health authorities recognize that long-term exposure can damage the body’s ability to produce healthy blood cells and can impair the immune system.
The Centers for Disease Control and Prevention (CDC) explains that long-term benzene exposure can decrease blood cell counts, contributing to anemia and increasing infection risk: findings that align with the way benzene is evaluated in occupational and environmental health investigations.
In most Benzene litigation, the dispute is not whether benzene is dangerous, but whether the exposure occurred at levels and durations that plausibly elevated a person’s cancer risk, and whether the medical record supports the claimed connection.
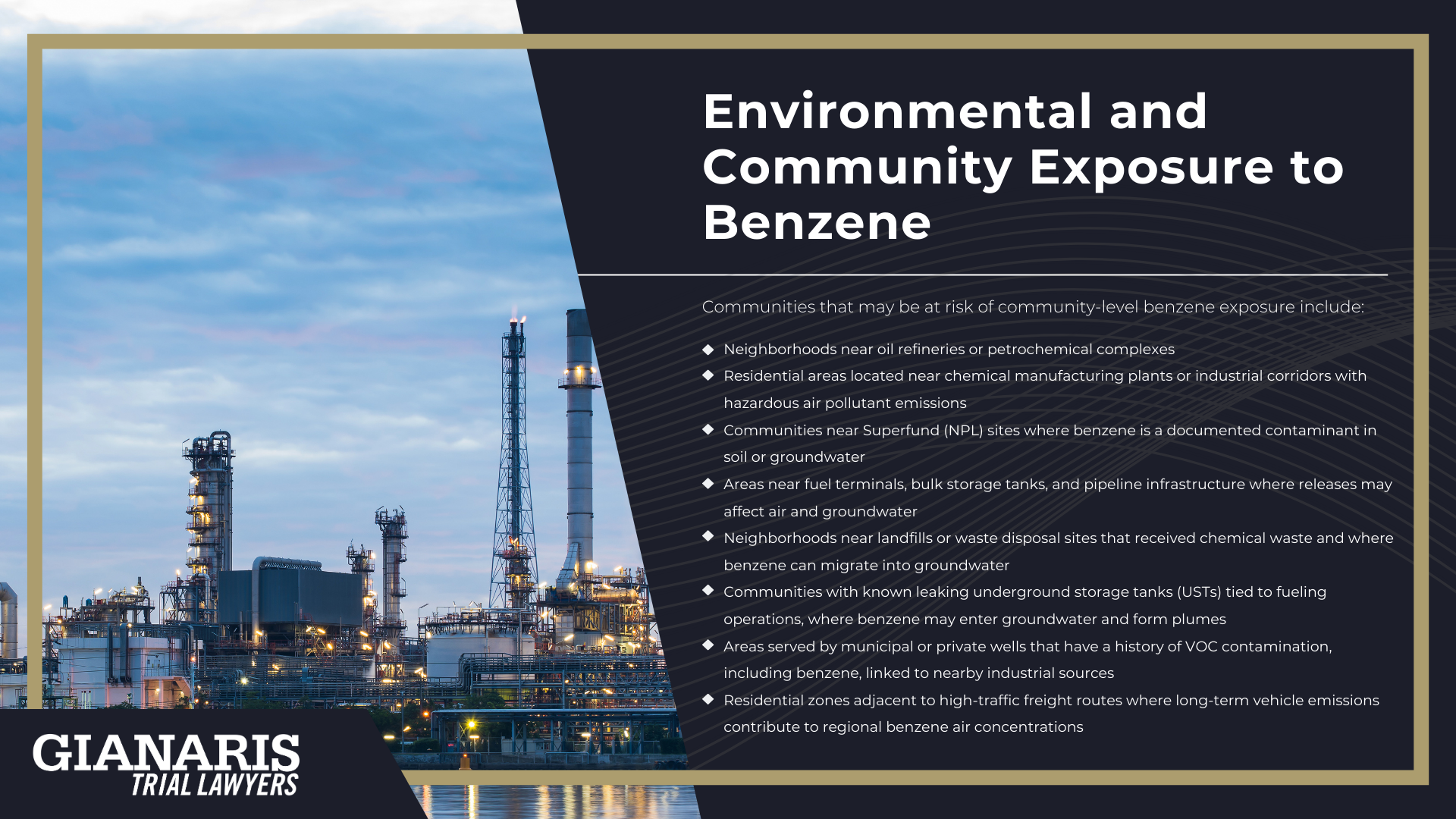
Regulators treat benzene as a cancer-causing air pollutant and a drinking-water contaminant because it appears frequently in industrial environments and contaminated sites.
For example, ATSDR notes that benzene has been detected at hundreds of EPA National Priorities List (Superfund) sites, which supports how often benzene appears in investigations involving toxic chemicals and environmental releases.
Eligibility also turns on how exposure is shown.
Many claimants were not handling benzene in laboratory-grade form; they were working around fuel vapors and industrial emissions where high Benzene levels can develop in enclosed or poorly ventilated areas.
Others were exposed through repeated skin contact with fuels or solvents, where liquid benzene or benzene-containing mixtures touched the skin as part of routine job duties.
The EPA’s own benzene health summary explains that benzene can affect bone marrow, cause excessive bleeding, and damage immune function through changes in blood cells and antibodies: biologic effects that often appear in the same cases where blood-related cancers are diagnosed.
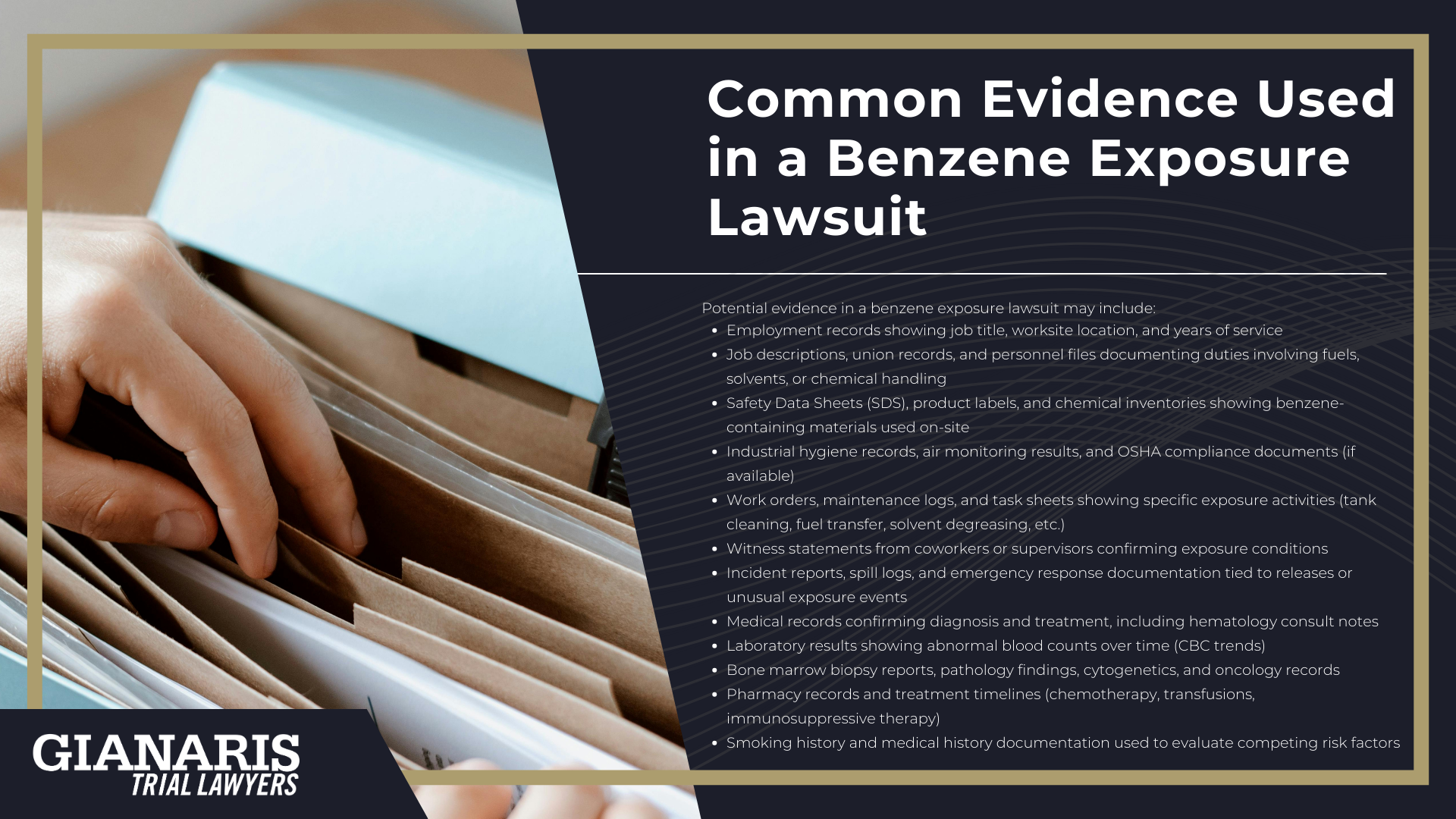
In practical terms, the core eligibility factors usually include:
- A clear exposure pathway showing how toxic exposure occurred (inhalation, skin contact, or contaminated water), including whether the person worked around fuels, solvents, or other toxic substances.
- Evidence of elevated exposure conditions, such as repeated work in areas where vapors accumulated, direct handling of benzene-containing products, or environmental releases tied to industrial operations.
- A diagnosis consistent with benzene-associated disease, most commonly leukemia and other blood-related cancers supported by medical records and pathology findings.
- Timing and latency consistency, meaning the medical diagnosis occurs within a timeframe that fits known patterns of benzene-related blood toxicity and leukemia development after sustained exposure.
- Documentation to support causation arguments, including employment records, exposure history, industrial monitoring data, or environmental testing where available.
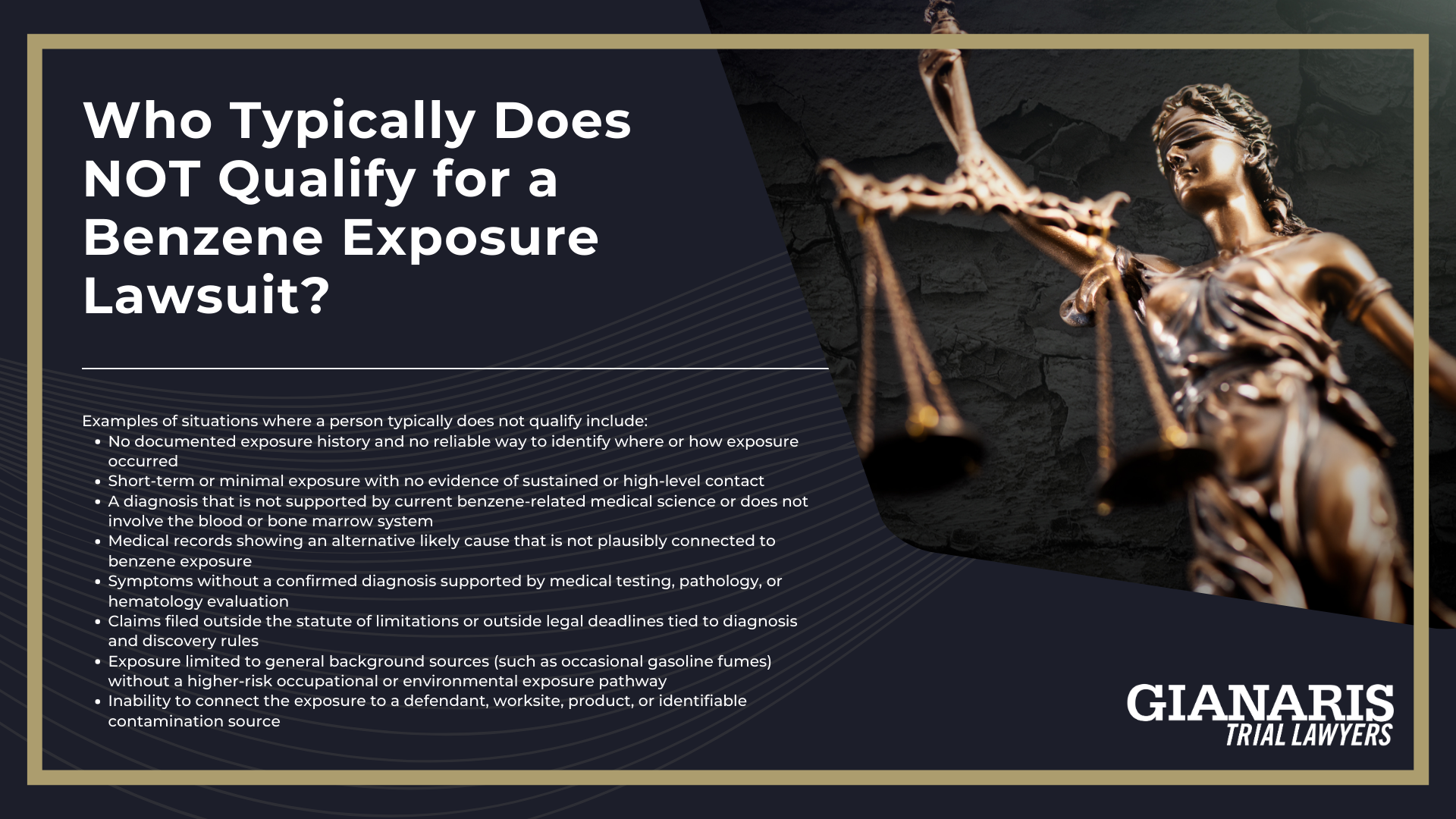
This framework explains why some claims qualify and others do not.
A person can have real exposure without meeting the legal and medical thresholds required to move forward, particularly when exposure was brief or cannot be documented.
At the same time, repeated exposure in work environments tied to fuels and industrial emissions can create the type of record that supports a claim, especially when serious blood or marrow disease appears afterward.
Federal regulators treat benzene as a high-concern pollutant in part because it is emitted by refineries and industrial facilities at scale, and the EPA has required controls and monitoring programs directed at benzene due to its role as a hazardous air toxic with carcinogenic properties.
Why Benzene Lawsuits Focus on Exposure History and Medical Diagnosis
Benzene lawsuits focus on exposure history and medical diagnosis because Benzene poisoning is primarily a blood and bone marrow injury, and the strongest scientific evidence connects benzene to disrupted blood cell production and leukemia.
OSHA’s benzene medical surveillance guidelines describe benzene as a hematopoietic toxin linked to pancytopenia, aplastic anemia, and leukemia, and they recognize both inhalation and skin absorption as important exposure routes, including contact with liquid benzene.
The National Toxicology Program, part of the Department of Health and Human Services, lists benzene as a human carcinogen and notes strong evidence tying it to myeloid leukemia, including acute myelogenous leukemia.
The World Health Organization (WHO), through IARC evaluations, has also concluded that occupational benzene exposure shows an increased risk of leukemia in exposed workers, which is why case screening often centers on blood cancers with documented latency.
Because benzene is present in petroleum products derived from crude oil, exposure scenarios often involve fuels, solvents, and industrial mixtures that also contain other chemicals, making a detailed work history important for isolating benzene as a meaningful contributor to the illness.
Exposure history also matters in environmental exposure cases tied to hazardous waste sites, where benzene contamination can persist in groundwater or air over long periods and may involve overlapping contaminant profiles.
The medical diagnosis is equally central because benzene-related diseases tend to follow recognizable clinical patterns, often beginning with blood abnormalities before progressing to leukemia, and public health agencies have also documented other systemic effects from sustained high exposure, including reproductive harm such as irregular menstrual periods in women exposed to high levels for extended periods.
Finally, because benzene is a component of tobacco smoke, defendants often argue alternative exposures, which is one reason case evaluation usually requires a clear timeline of when and how the exposure occurred and whether the diagnosis fits known benzene carcinogenic risks.