Chronic obstructive pulmonary disease (COPD) is a broad term for lung and airway diseases that limit airflow because of damage in the airways and/or the lung’s air sacs (alveoli).
Cleveland Clinic describes COPD as involving airway inflammation and scarring, damage to the air sacs, or both, most often in the forms of chronic bronchitis and emphysema.
The Centers for Disease Control and Prevention (a U.S. Department of Health and Human Services agency) reports that COPD remains common in the United States; in 2023, the age-adjusted prevalence of diagnosed COPD in adults was 3.8% (NHIS data).
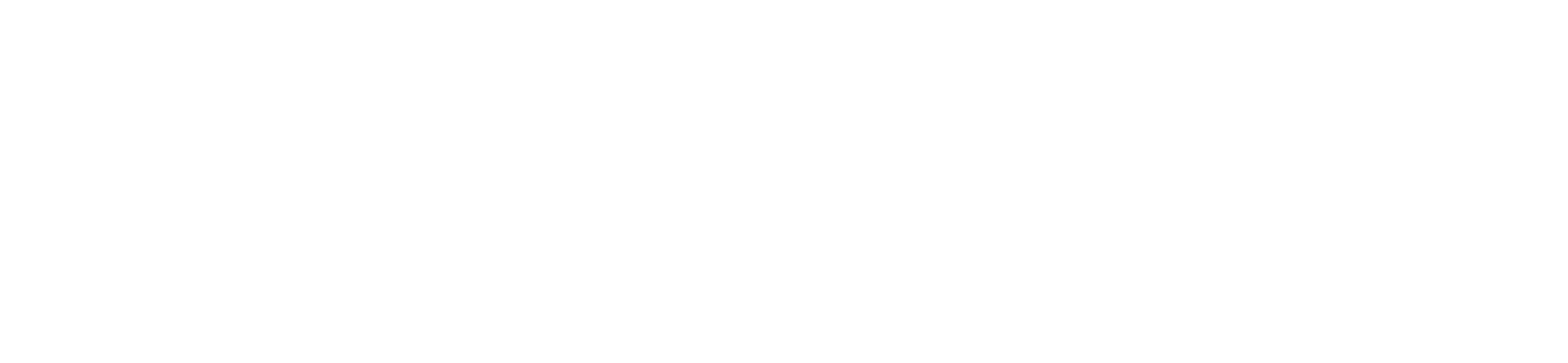
COPD is strongly associated with long-term inhalation of lung irritants, and the National Heart, Lung, and Blood Institute (NIH) lists chronic exposure to air pollution, chemical fumes, and dust from the environment or workplace among factors that can raise the likelihood of developing COPD.
COPD also places people at higher risk for complications from respiratory infection, which is why preventive care is routinely part of COPD management.
High-level COPD overview (and what it’s linked to):
- A disease defined by obstructed airflow: COPD is characterized by persistent airflow limitation driven by airway and/or alveolar abnormalities.
- Inflammation and structural damage: COPD is tied to chronic airway inflammation and scarring and/or destruction of the air sacs (alveoli).
- Linked to long-term irritant exposure: Beyond smoking, NHLBI identifies long-term exposure to air pollution, workplace chemical fumes, and dust as key non-smoking risk contributors for developing COPD.
- Related to (but distinct from) reactive airway disease: COPD is a chronic obstructive condition; reactive airway disease is sometimes used as a non-specific label for asthma-like airway reactivity, and the clinical workup focuses on separating asthma/reactive patterns from fixed obstruction seen in COPD.
- COPD prevalence is tracked nationally: CDC surveillance commonly measures COPD based on whether adults have been told they have COPD, emphysema, or chronic bronchitis, reflecting how the condition is diagnosed and reported.
- Higher infection risk and vaccine prevention: MedlinePlus notes that people with COPD are at higher risk for serious problems from infections like influenza and pneumococcal pneumonia, and vaccination is a standard preventive recommendation in COPD care.
- Pulmonary rehabilitation as core management: Pulmonary rehabilitation is a medically supervised program used for chronic lung diseases like COPD, focused on improving function and teaching disease-management strategies.
- Oxygen therapy for advanced disease states: Oxygen therapy may be prescribed when COPD leads to low blood oxygen levels, as part of supportive treatment planning.
COPD Symptoms and Daily Impact
COPD affects how air moves in and out of the lungs, leading to poor airflow and reduced lung function as the disease takes hold.
The condition damages the tiny air sacs responsible for oxygen exchange and narrows inflamed airways, which explains why difficulty breathing becomes a defining feature over time.
For many people, symptoms begin gradually and may be mistaken for aging or reduced fitness, especially when early changes feel manageable.
As airflow limitation worsens, daily activities require more effort and recovery time, even without exertion.
In advanced cases, long-term strain on the heart and lungs can contribute to complications such as pulmonary hypertension, significantly affecting overall health.
Common symptoms and impacts of COPD include:
- Mild symptoms early on, such as shortness of breath with exertion or fatigue during routine tasks
- More mucus production that contributes to chronic cough and airway blockage
- Chest tightness caused by airway narrowing and persistent inflammation
- Difficulty breathing during activity or at rest as airflow becomes increasingly restricted
- More severe symptoms over time, including reduced stamina, frequent respiratory infections, and limitations on work and daily independence
How COPD Progresses Over Time
COPD is a chronic condition that typically becomes progressively worse as lung damage accumulates and airflow limitation increases.
In the early stages, symptoms may be mild, which can delay diagnosis and allow inflammation and structural changes in the lungs to continue unchecked.
Over time, narrowing airways and damaged air sacs make it harder to move oxygen into the bloodstream, placing added strain on the heart and increasing the risk of complications such as heart disease.
As oxygen levels fall, some people eventually require supplemental oxygen to maintain basic organ function and tolerate daily activity.
Although smoking is often cited as the biggest risk factor, ongoing occupational exposures and environmental irritants can continue to drive disease progression even after smoking stops or in individuals who never smoked.
Early treatment can slow decline by improving airflow, helping reduce inflammation, and limiting the frequency of flare-ups that accelerate lung damage.
Without effective management, repeated exacerbations may lead to rapid loss of lung function and increased hospitalizations.
Understanding how COPD progresses underscores why early diagnosis and exposure control matter for long-term health and quality of life.