Railroad employees faced daily contact with toxic agents that medical science now recognizes as major risk factors for laryngeal cancer.
Workers were regularly exposed to diesel exhaust, which filled locomotive cabs, switch yards, and repair shops with soot and polycyclic aromatic hydrocarbons (PAHs).
At the same time, many repair facilities contained asbestos insulation and locomotive parts manufactured with asbestos, releasing fibers into the air whenever brakes, gaskets, or insulation were cut or replaced.
Decades of research confirm that asbestos exposure, especially with prolonged exposure, significantly increases the risk of cancers of the larynx.
Shop crews also may have handled strong acid mists, welding fumes, and solvents: dangerous substances that compounded risk by irritating and damaging the lining of the throat over time.
Studies have shown that this combination of exposures created an elevated risk of developing cancer of the larynx, particularly for employees with long years of service in rail shops or on the tracks.
Unlike bursts of short-term exposure, the chronic accumulation of inhaled fibers, soot, and chemicals led to a gradual but profound health impact.
These exposures often went unchecked because railroad companies failed to provide protective gear or implement ventilation systems, even after the dangers of asbestos and diesel exhaust exposure were well documented.
As a result, many workers developed cancers that shortened their life expectancy and left them with debilitating complications.
Toxic Chemicals in Railroad Work Linked to Laryngeal Cancer
A laryngeal cancer diagnosis among railroad employees is rarely the result of a single toxin.
Instead, it reflects years of contact with multiple hazardous substances in the rail industry that damaged the respiratory tract and created lasting health risks.
Workers have been exposed to diesel exhaust, asbestos, solvents, and PAHs from creosote-treated railroad ties, often without warnings or protective equipment.
These exposures contributed to both immediate respiratory irritation and the long-term development of serious occupational illness.
Research has repeatedly shown that the combination of diesel exposure, benzene exposure, and other dangerous substances significantly increases cancer risk in transportation and industrial settings.
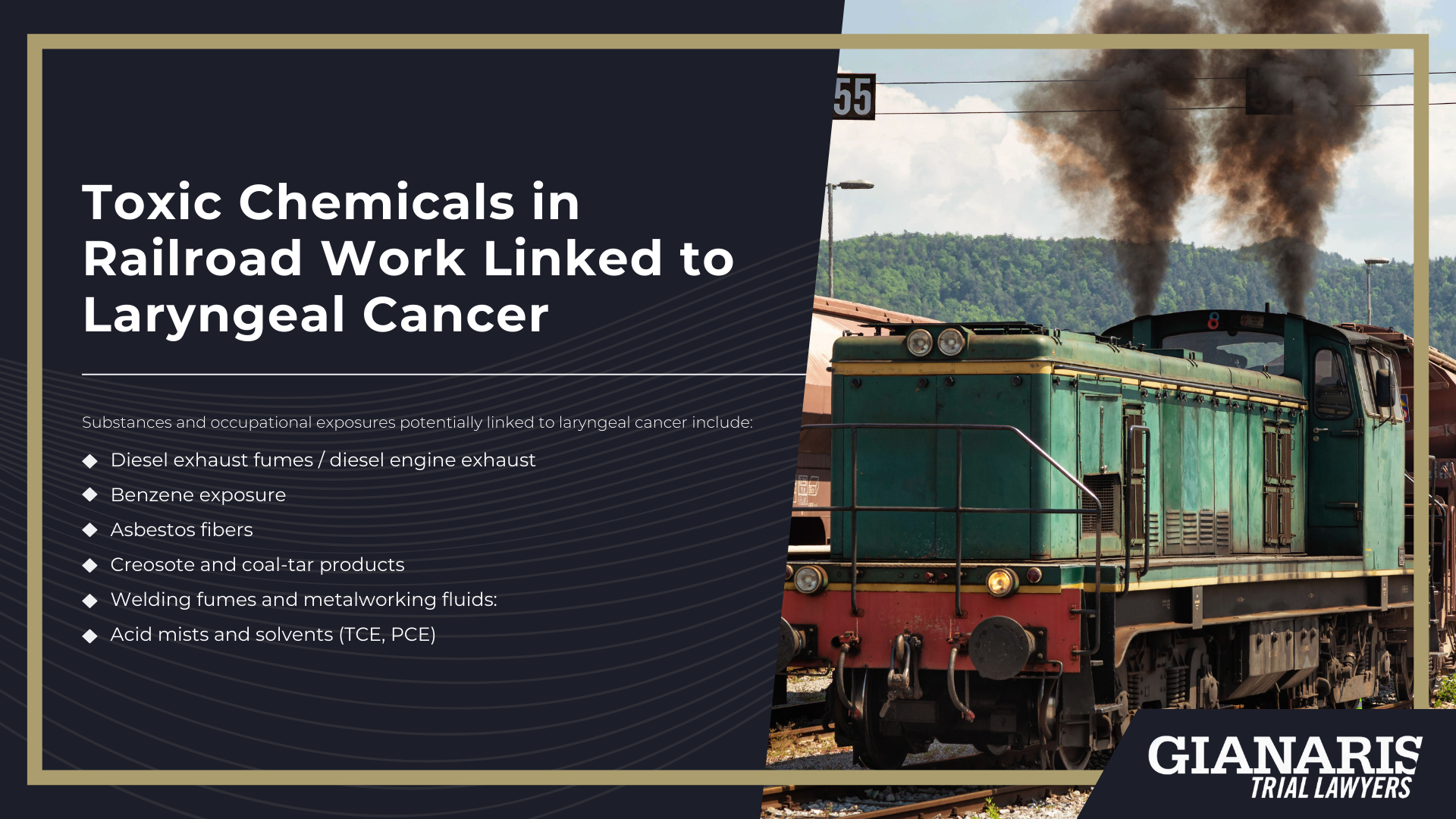
Substances and occupational exposures potentially linked to laryngeal cancer include:
- Diesel exhaust fumes / diesel engine exhaust: A constant hazard in locomotive cabs, yards, and shops, containing PAHs, nitro-PAHs, and fine particulates that irritate and damage the larynx over years of diesel fuel combustion.
- Benzene exposure: Present in fuels, lubricants, and solvents used throughout the railroad industry; known to cause cancer and implicated in upper aerodigestive tract malignancies.
- Asbestos fibers: Released from locomotive parts manufactured with asbestos and asbestos insulation, with clear evidence linking asbestos to laryngeal cancer.
- Creosote and coal-tar products: Applied to railroad ties and timbers, containing PAHs that damage the lining of the esophagus and larynx.
- Crude oil vapors: Encountered by workers handling tank cars or maintaining pipelines, creating inhalation risks tied to head, neck, and throat cancers.
- Welding fumes and metalworking fluids: Sources of other dangerous substances, including heavy metals and particulates that increase upper respiratory cancer risks.
- Acid mists and solvents (TCE, PCE): Common in shop cleaning and degreasing, causing chronic irritation and long-term cellular damage in the larynx.
These exposures often overlapped, meaning exposed workers experienced cumulative risk over decades of service.
Whether through constant diesel fuel combustion, chronic asbestos dust, or crude oil vapors, the combined effects created a profound elevated risk for throat and voice-box cancers.
For many, the connection between railroad duties and a laryngeal cancer diagnosis only became clear years later, underscoring the preventable nature of these occupational illnesses.
Scientific Studies on Laryngeal Cancer and Occupational Exposures
The larynx sits at the crossroads of air and particle flow, so exposures common in rail settings (diesel combustion products, asbestos, strong acid mists from battery rooms, welding fumes, and PAH-rich creosote/coal-tar) are directly relevant.
The most authoritative, rail-applicable evidence for laryngeal cancer is strongest for asbestos and strong inorganic acid mists containing sulfuric acid; there is also a credible signal for polycyclic aromatic hydrocarbons (PAHs) from combustion and creosote.
Evidence for diesel exhaust at the larynx specifically is mixed (clear for lung cancer, weaker for larynx), while welding/metalworking exposures are Group-1 carcinogens overall with head-and-neck signals in cohort and case-control work.
Together, these findings help explain how multi-agent, long-duration railroad exposures can culminate in laryngeal cancer decades after employment ends.
Studies on occupational exposures related to laryngeal cancer include:
- IARC & National Academies on asbestos (causal for larynx): The IARC re-evaluation concluded there is sufficient evidence in humans that asbestos causes cancer of the larynx; pooled cohort data show RR ≈ 1.4 for “any” exposure, higher at the top exposure strata. The U.S. Institute of Medicine independently reached the same causal conclusion in Asbestos: Selected Cancers.
- Strong inorganic acid mists (sulfuric acid): The U.S. NTP profile and NCI overview identify laryngeal cancer as a target site; the classic U.S. steel-pickling cohort reported about a two-fold excess of laryngeal cancer after adjustment for smoking, with confirmation on extended follow-up. This maps to battery-charging/acid-mist tasks in rail shops.
- PAHs from combustion/creosote: A systematic review and meta-analysis in Occupational & Environmental Medicine found a positive association between occupational PAH exposure and laryngeal cancer; toxicology profiles document PAH richness in diesel exhaust and creosote/coal-tar, consistent with rail tasks (ties, yards).
- Welding fumes / metal fabrication: IARC reclassified welding fumes as Group 1 carcinogenic (based on lung); large case-control work in the French ICARE study evaluated head-and-neck subsites (including the larynx) in relation to welding exposure, supporting treatment of welding as a meaningful co-exposure in shops.
- Metalworking fluids (MWFs): Auto-manufacturing cohorts and nested case–control analyses of upper aerodigestive tract cancers (which include laryngeal sites) reported increased risks with long-term MWF exposure, an exposure pattern analogous to machinist/grinding roles in rail shops.
- Diesel exhaust at the larynx (mixed): A modern analysis from the ICARE program examining diesel motor exhaust and oral/pharyngeal/laryngeal cancer did not show a clear positive association; an older hospital-based case-control on “diesel fumes” likewise failed to find a robust link. These results indicate that, for laryngeal cancer specifically, diesel should be framed as part of cumulative, multi-agent exposure rather than a sole driver (in contrast to its established role in lung cancer).
What Railroad Jobs are at the Highest Risk of Laryngeal Cancer?
Laryngeal cancer risk rises in roles where workplace exposures stack up, especially chronic exposure to diesel exhaust, welding fumes, PAH-rich creosote, acid mists from battery rooms, and dust from legacy insulation.
Shop crafts and operating crews often spent long shifts in enclosed or poorly ventilated spaces, multiplying dose over years.
In many facilities, routine maintenance meant inhaling asbestos fibers released from brakes, gaskets, and insulation on older equipment, while track work brought creosote, herbicides, and diesel-powered machinery into close contact.
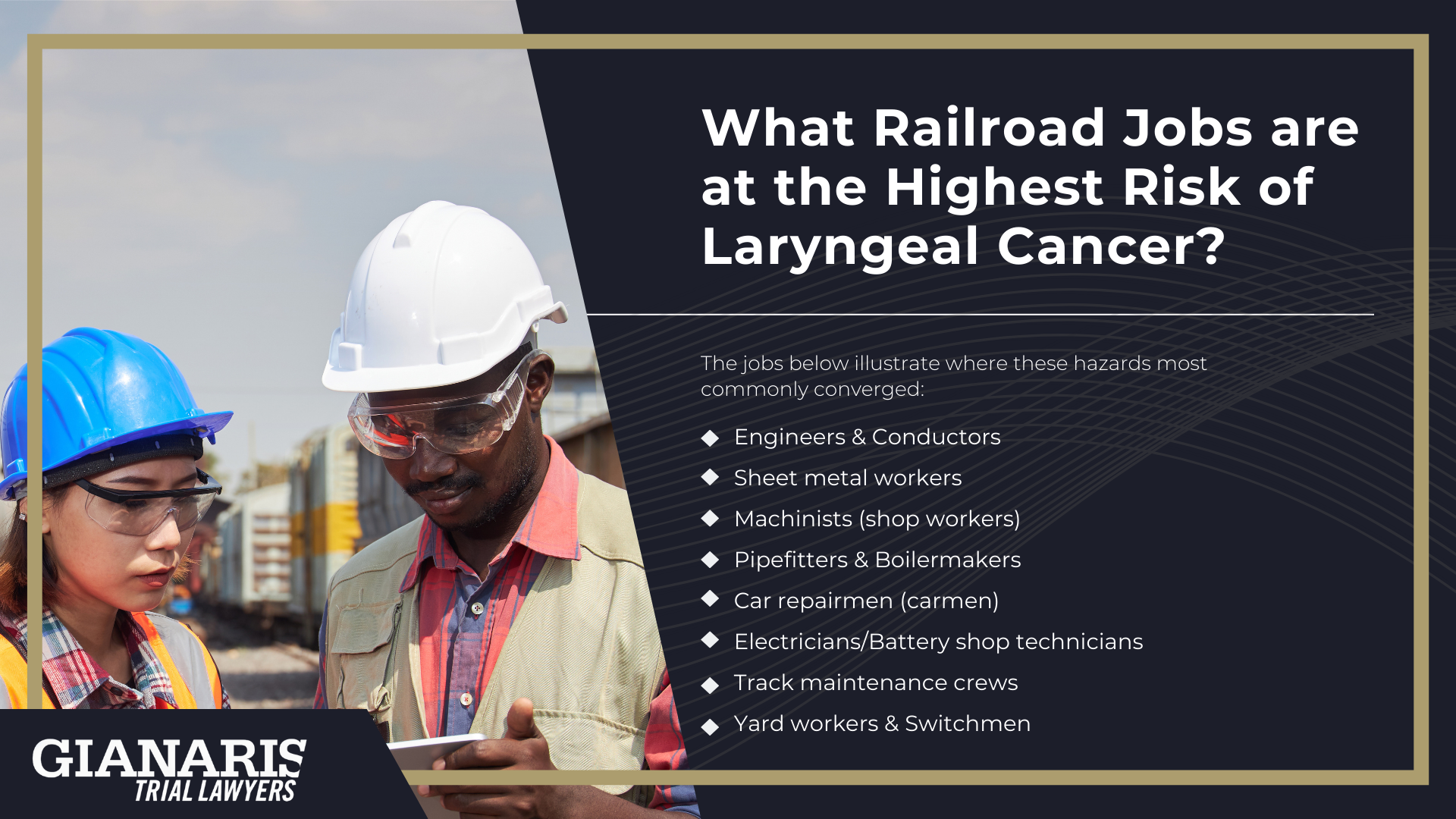
The jobs below illustrate where these hazards most commonly converged:
- Engineers & Conductors: Continuous exposure to diesel exhaust in locomotive cabs and yards; PAH-laden soot and fumes across long, cumulative shifts.
- Sheet metal workers: Cutting, grinding, and welding of car and engine components; heavy welding fume loads, occasional contact with legacy lagging/insulation.
- Machinists (shop workers): Metalworking fluids, solvents/degreasers, welding fumes, and brake/gasket work that could mean inhaling asbestos fibers.
- Pipefitters & Boilermakers; Isulation and gasket removal/installation on engines and boilers; heat and steam work that disturbed asbestos and emitted fumes.
- Car repairmen (carmen): Brake and clutch service (historic asbestos sources), paints/solvents, and frequent diesel emissions around train cars in shops.
- Electricians/Battery shop technicians: Strong inorganic acid mists during charging/maintenance; confined areas that amplify inhalation dose.
- Track maintenance crews: Creosote-treated railroad ties, ballast dust/silica, herbicides, and diesel equipment—sustained outdoor exposure with intermittent high peaks.
- Yard workers & Switchmen: Constant yard-level diesel exhaust from idling locomotives and switching operations; repetitive, cumulative fume contact.
These roles don’t act in isolation; many workers rotated through tasks that combined multiple hazards over decades.
That overlap (diesel, welding, creosote, solvents, acid mist, and asbestos) creates a powerful exposure narrative for laryngeal cancer in railroad employment.
Can Family Members File a Wrongful Death Claim if a Loved One Passed Away from Laryngeal Cancer?
Yes, family members can pursue a wrongful death claim if a loved one developed laryngeal cancer as a result of toxic exposures during railroad work.
These claims recognize that long-term exposure to diesel exhaust, asbestos, welding fumes, or other hazardous agents often plays a significant role in causing the disease.
Importantly, a worker’s employment status at the time of diagnosis, whether retired, active, or long since separated from the railroad, does not prevent families from seeking justice.
Wrongful death claims may provide compensation for medical expenses, lost income, and loss of companionship.
They also hold railroad companies accountable for unsafe environments that left generations of workers at elevated risk.
By connecting medical records with documented workplace hazards, families can demonstrate how preventable occupational conditions led to a devastating loss.